We are living in extraordinary times, with a novel coronavirus (2019-nCoV) outbreak that has become a public health emergency of international concern. This affects us all. The Olympic Games have been postponed, as have all other sporting events. Unemployment, bankruptcies, economic collapse, hospitals overrun, and many lives lost already.
While performance and training is the hallmark of our passion at HIIT Science, we are taking a pause on specific HIIT Science posts to highlight an important but often overlooked contributor to the current crisis – the overfat condition.
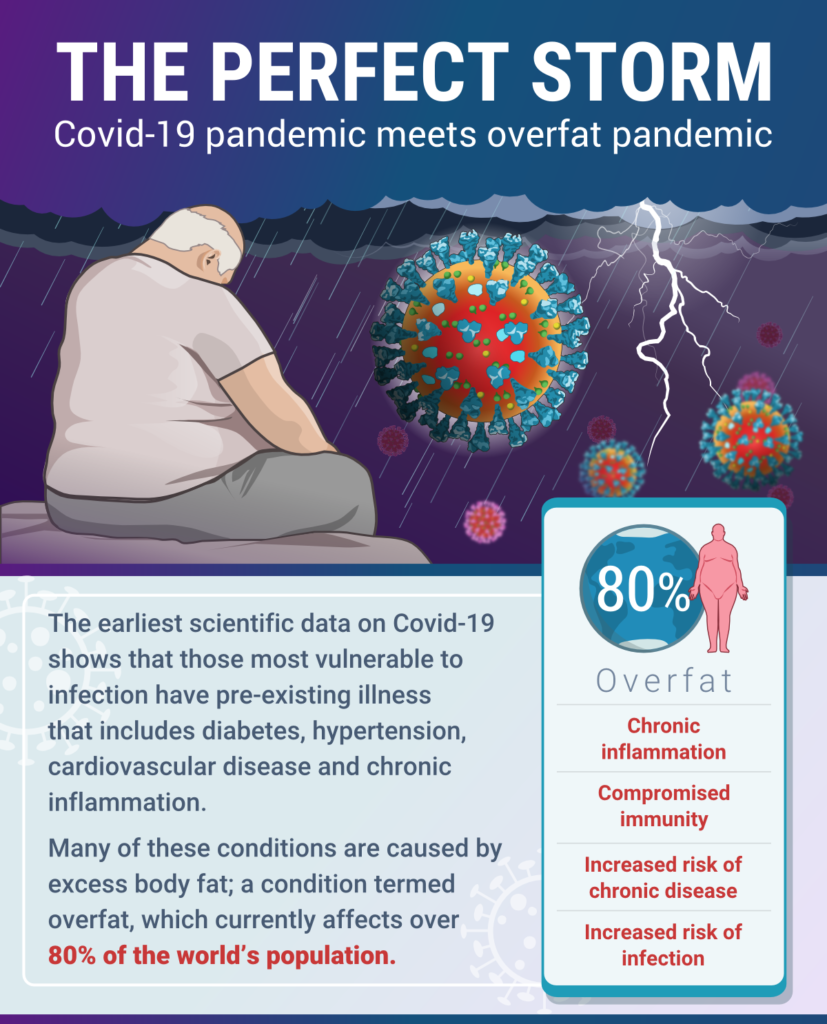
The collision of the Covid-19 pandemic with the prevailing overfat pandemic is what
Philip Maffetone and I recently termed “The Perfect Storm”. In
our paper, published in this month’s issue of Frontiers in Public Health, we highlight the importance of healthy body fat levels to support optimal immune function, lowered risk of chronic disease, and reduced risk of infection – including coronavirus.
Our hope is that by appreciating one of the underlying contributors to the pandemic we can all become part of the solution for future viral outbreaks.
What is Overfat?
As a reader, you’re probably more aware of the term overweight and obese. These are mainstream terms used by most scientists and practitioners. The terms, which stem from the
body mass index (BMI), provide cut-offs that place a person into their category. Using an individual’s weight in kilograms divided by their height in meters squared, standardized cut-off points indicate the clinical diagnoses of being underweight, of normal weight, overweight, or obese, according to the following categories (in kilograms per square meter):
- <18.5 = underweight
- 18.5–24.9 = normal weight
- 25–29.9 = overweight (pre-obese)
- >30 = obese.
However, those of us who actually do the measurement and the math, especially with many of our muscular and healthy athletes, soon discover that they fall into the overweight (and sometimes even obese) categories according to this formula. Something is obviously wrong. This highlights the inaccuracy of the method and the need for
new assessments and terms (see Figure 1).
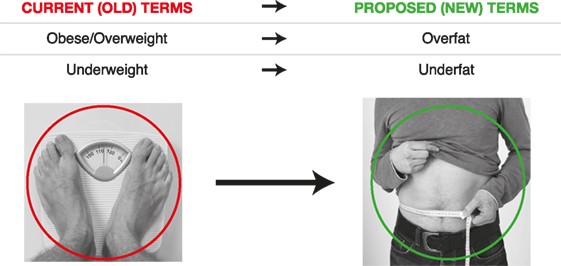
Figure 1. Comparison between current terms and proposed terms
As we always say in HIIT Science, we need to measure what matters.
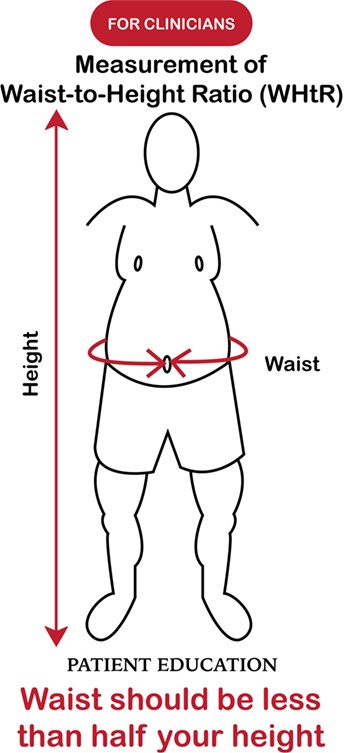
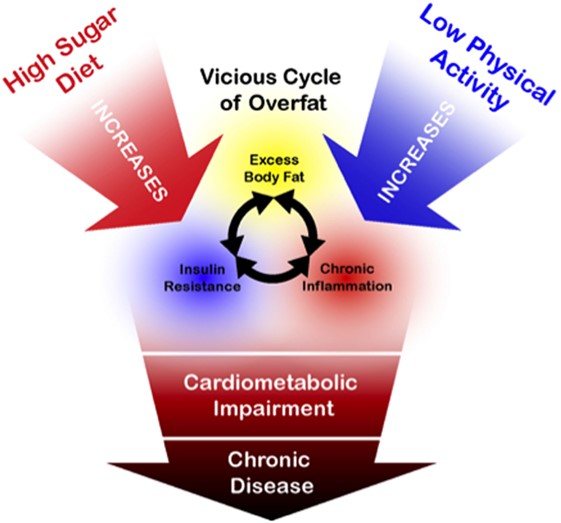
So, what matters here in the context of health? It’s the level of visceral fat or tummy fat a person carries. When this level is inappropriate, it is the sign of being
overfat – or the state of having excess body fat that impairs health. How can one measure that? As we teach in HIIT Science (Chapter 7), we measure the waist to height ratio – your waist should be less than half your height (see Figure 2 below).
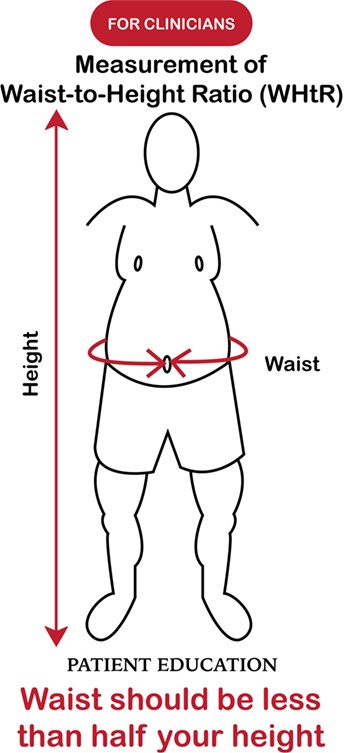
Figure 2. Measurement of waist to height ratio to assess overfat
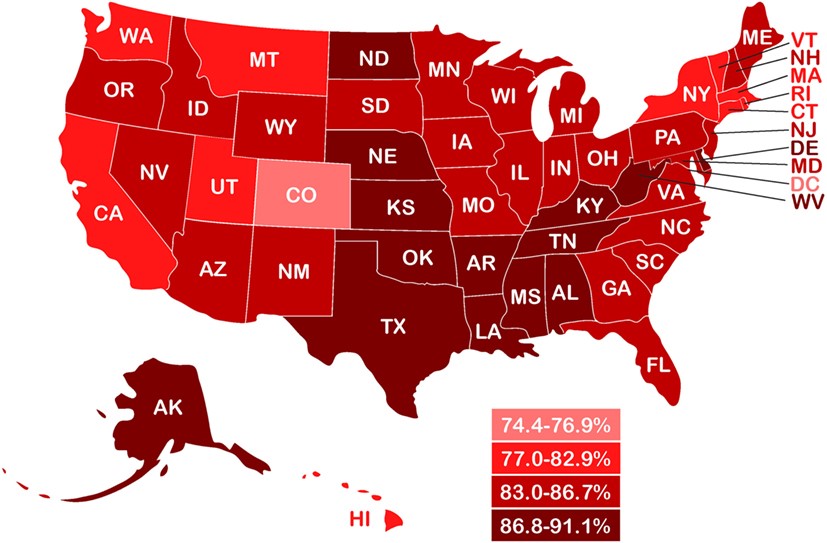
Billions of people across the globe are
overfat, some unknowingly as it does not just affect those that hit the obesity or overweight BMI cutoffs. In fact,
shocking recent estimates suggest that over 80 percent of adults in the world may be overfat. These figures are worrying in the wake of the current COVID-19 pandemic, since overfat and its
resultant comorbidities have shown
poorer clinical outcomes in patients with COVID-19. Comorbidities include diabetes, hypertension, and heart disease, all of which are associated with the condition of being overfat. Warnings have emerged already from the
UK,
France and the
US.
What evidence is there to support being overfat as a risk factor for COVID-19?
Following the 2009 swine flu (H1N1) pandemic, it was discovered that obesity was an independent risk factor for infection and mortality. During this COVID-19 pandemic, a similar pattern has emerged already. Compare the recent cases in New York and New Orleans as one example. On a per capita basis, New Orleans has had at least 7x more cases than New York, with a death rate that is also
2x higher. Statistics show that many New Orleans residents are prone to be overfat and have related illnesses including diabetes and hypertension, at rates higher than the national average; conditions that can make patients more vulnerable to COVID-19. The
most recent CDC data shows that approximately 90% of hospitalized patients with COVID-19 had one or more underlying conditions associated with being overfat.
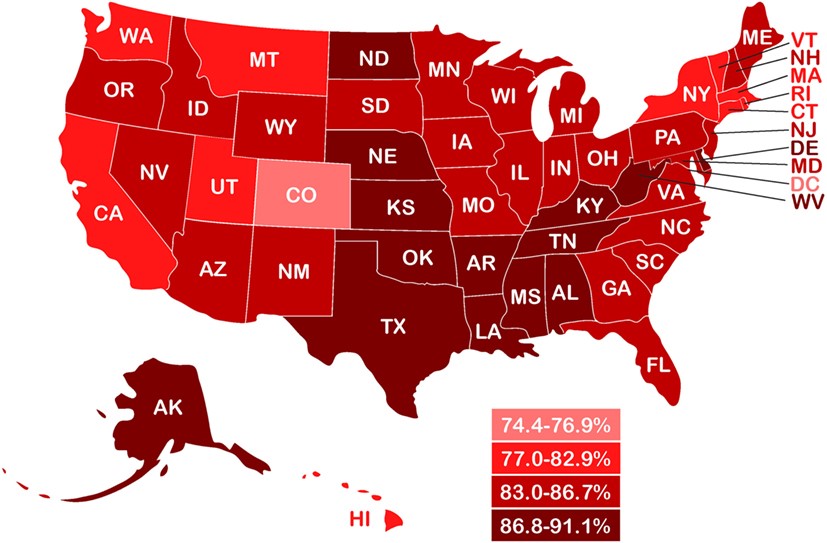
Figure 3. State-by-state estimated prevalence of overfat adults (2013–14) based on reported prevalence of overweight and obesity. From Maffetone & Laursen (2017).
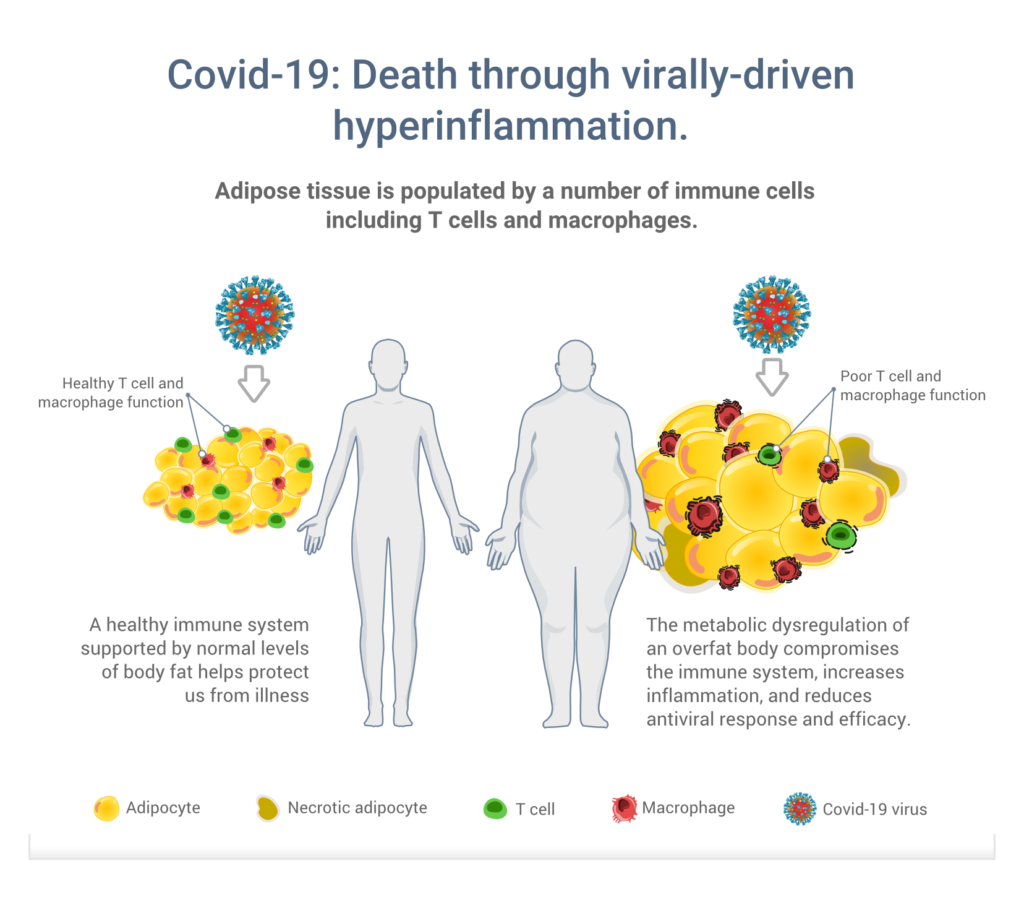
More than 10 years on from the swine flu pandemic, we now know that having excess fat, particularly in the abdominal area, can impair immune function and overall health. Why? Excess body fat contains numerous different immune cells that, unlike healthy fat, do not function properly to protect the body against infection. Figure 4 below, which appears in
our paper, gives us a summary of the issue and the importance of having normal (healthy) levels of body fat.
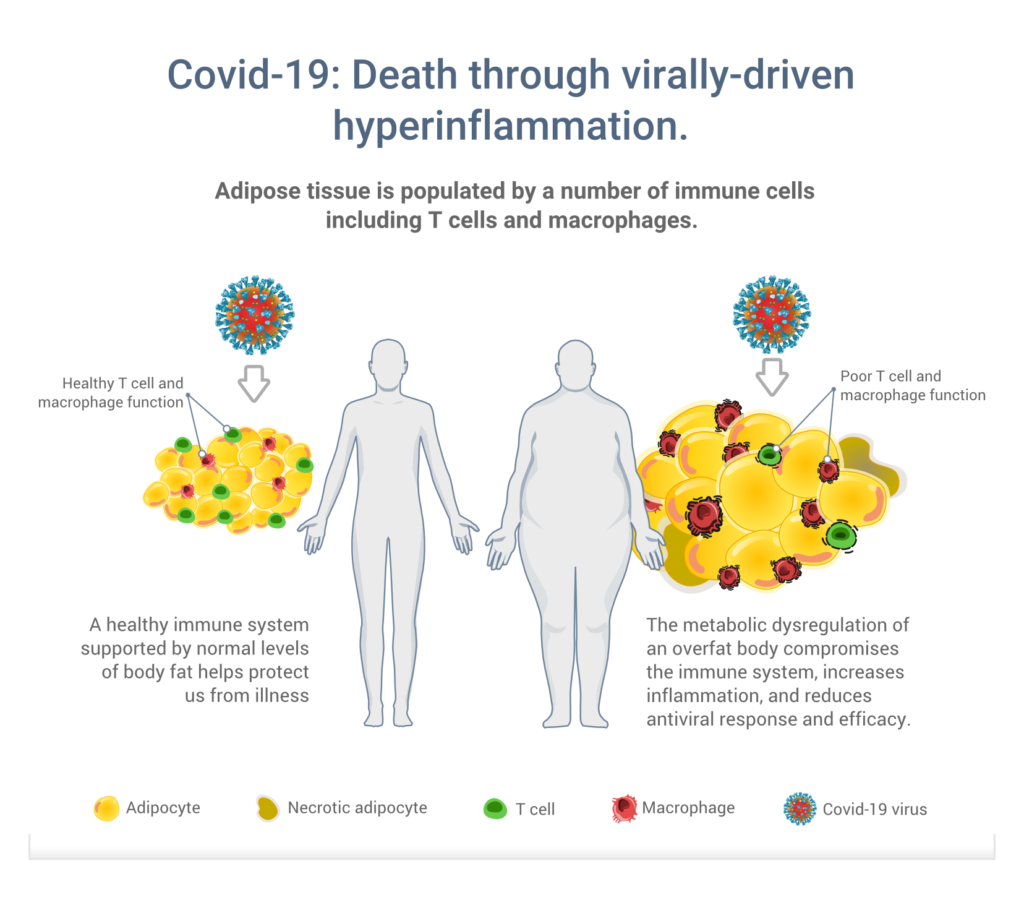
Figure 4. Role that fat cells play in the metabolic (dys)regulation and support of the immune system. From Maffetone & Laursen (2020).
For more information about the increased risk of infection from being overfat, check out Chapter 7 of the HIIT Science book or online course, written by Dr Maffetone.
How healthy lifestyle behaviours will help to reduce the future risk of infection
As the old adage goes, “hindsight is always 20/20”. Echoing the voices of
David Ludwig and Richard Malley in this crisis, what should be clear now is that it would be easier to prevent severe viral infections like COVID-19 than to treat them. In the short term, individuals and governments must practice current mitigation strategies such as hand hygiene, respiratory etiquette, and safe social distancing. In the future however, we need to focus more on improving overall health, including lowering the incidence of being overfat. While testing for COVID-19 remains elusive, individuals can test for being overfat simply by measuring waist circumference (Figure 2). However, it is also important that a person is not underfat, as this too increases the risk of viral infection (Figure 5).
If you discover that you may be overfat or underfat, speak with your healthcare provider about the best steps to take. For everyone, no matter what your fat status, there are strategies you can employ at home in order to improve your immune system function. Eliminating sugar and increasing activity levels, for example by walking more, or incorporating a low impact HIIT session, is just one approach.
See our post about indoor HIIT solutions for some session ideas. Figure 6 provides a summary of some of the key behaviours that contribute to excess body fat, chronic disease, and compromised immunity.
For more information, and to give yourself the tools to land in the healthy normal fat levels,
we are offering Chapter 7, ‘Health and HIIT’ completely free! This offer is only available for a limited time. This is our most popular short course product, packed full of information on how to be healthy. The coupon code for the course is: PERFECTSTORM. If you want more information, please subscribe to our newsletter
HERE.
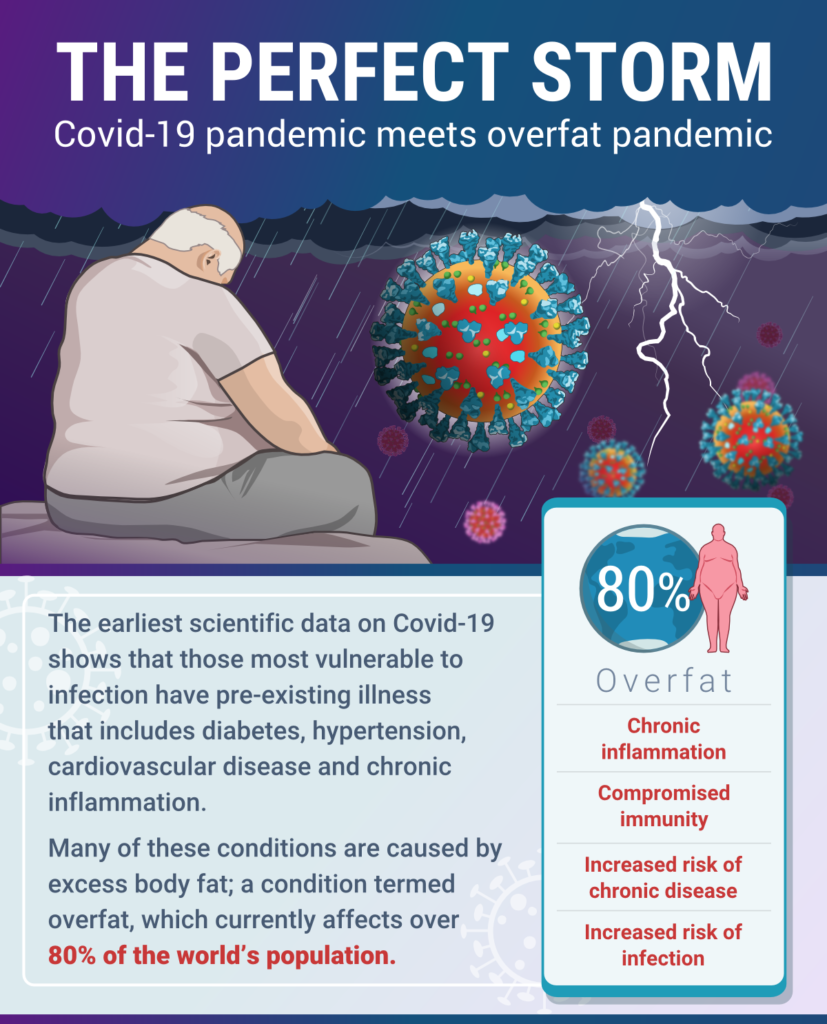 The collision of the Covid-19 pandemic with the prevailing overfat pandemic is what Philip Maffetone and I recently termed “The Perfect Storm”. In our paper, published in this month’s issue of Frontiers in Public Health, we highlight the importance of healthy body fat levels to support optimal immune function, lowered risk of chronic disease, and reduced risk of infection – including coronavirus.
The collision of the Covid-19 pandemic with the prevailing overfat pandemic is what Philip Maffetone and I recently termed “The Perfect Storm”. In our paper, published in this month’s issue of Frontiers in Public Health, we highlight the importance of healthy body fat levels to support optimal immune function, lowered risk of chronic disease, and reduced risk of infection – including coronavirus.